Periodontal disease is a serious oral health concern and is a leading cause of tooth loss around the world. A number of medical conditions are associated with periodontal disease and this article will focus on 3 conditions: diabetes, atherosclerosis and hormone imbalance. This article explores each of these conditions and their implications for your oral health.

In this article, we will delve into three medical conditions that are closely linked to periodontal disease: diabetes, atherosclerosis, and hormone imbalance. Periodontal disease is a major cause of tooth loss and this can be a serious oral health concern, impacting not only your ability to chew and speak but also your overall quality of life.
Understanding the connection between these medical conditions and periodontal disease is crucial for proactive prevention and effective management. Let’s explore each of these conditions and their implications for your oral health.
Diabetes and Periodontal Disease
The Relationship Between Diabetes and Periodontal Disease
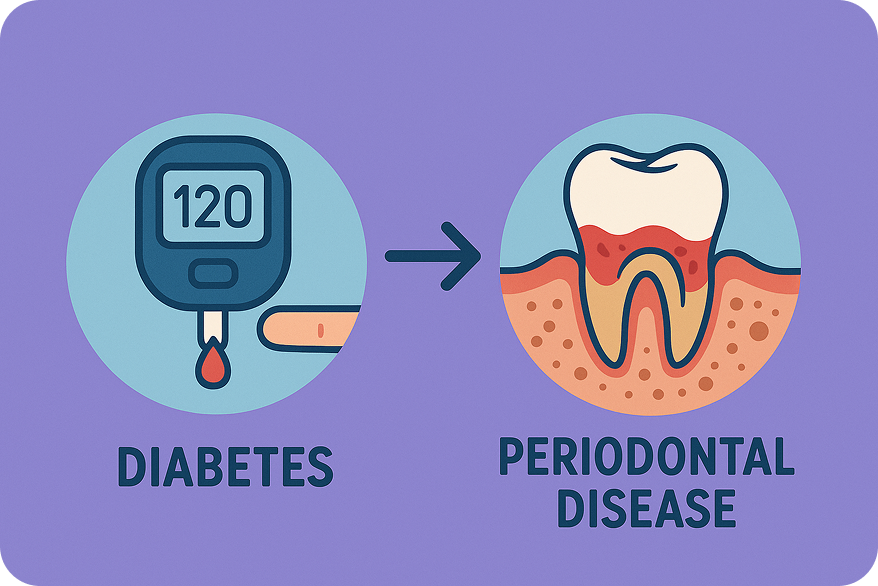
Diabetes is a disease of disrupted glycemic control resulting from a lack of insulin production (type 1) or systemic insulin resistance (type 2). Prolonged elevation of blood sugar (hyperglycemia) is the primary cause of the numerous complications created by diabetes. This includes negative effects on the heart, eyes, kidneys and peripheral nerves. Studies suggest that periodontal disease is a major complication of diabetes. Individuals with diabetes have at least a 3 times greater risk of periodontal disease than those without diabetes.
How does diabetes cause periodontal disease? Prolonged hyperglycemia results in increased inflammation of the tissues surrounding the teeth. This can lead to severe gum inflammation and loss of bone around the teeth (periodontal disease). Loss of bone that supports the teeth is a leading cause of tooth loss.
Moreover, diabetes-related inflammation and compromised immune function can hinder the body’s ability to combat oral infections. As a result, individuals with diabetes are more susceptible to dental issues, which can ultimately lead to tooth loss if left unaddressed.
A recent article from The American Dental Association concluded that US adults with uncontrolled diabetes and controlled diabetes were more likely to experience tooth loss than adults without diabetes.
Prevention and Management
To prevent tooth loss in diabetic patients, maintaining optimal blood sugar control is paramount. Consistently monitoring and managing blood glucose levels through a well-balanced diet, regular exercise, and prescribed medications or insulin can significantly reduce the risk of oral complications.
Regular dental check-ups are equally vital in preventing gum disease and tooth loss. Dentists can closely monitor the oral health of diabetic patients and provide timely interventions when needed. Additionally, meticulous oral hygiene practices, such as brushing, flossing, and using an antiseptic mouthwash, are essential for managing the risk of gum disease.
Diabetic individuals should actively collaborate with their dentist to create a customized oral care plan that considers their specific needs. This tailored approach to oral health can help address the heightened risks associated with diabetes, ultimately safeguarding their teeth and promoting a healthier smile.
Atherosclerosis and Periodontal Disease
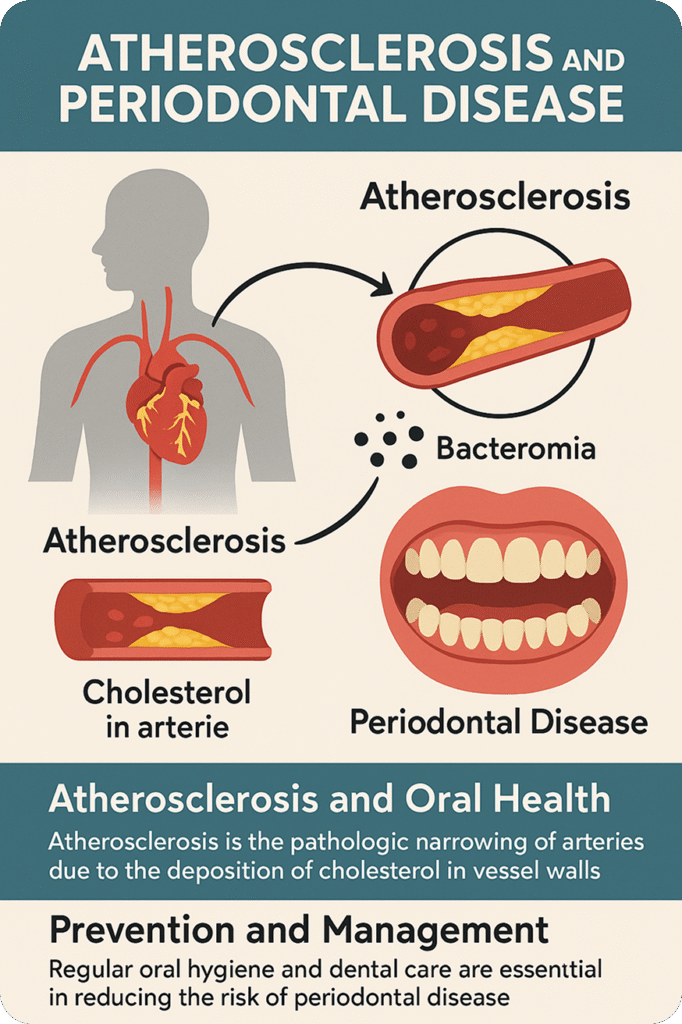
Atherosclerosis and Oral Health
Atherosclerosis is the pathologic narrowing of arteries due to the deposition of cholesterol in vessel walls. It is the primary cause of most cases of coronary heart disease and stroke. Many studies have shown that patients with a history of heart attack and stroke have worse oral health than healthy individuals.
How does poor oral hygiene contribute to heart attack and stroke? Patients with periodontal disease and poor oral hygiene suffer from frequent severe gingival inflammation and circulation of bacteria in the bloodstream (bacteremia). This bacteremia activates the body’s inflammatory response leading to injury of the vascular walls of the arteries. Injury to the walls of the arteries leads to narrowing and plays a major role in causing heart attacks and strokes.
Many studies have demonstrated that periodontal disease has a strong association with the risk of coronary artery disease and heart attack. There are also other studies that have not shown this link. Currently, there is insufficient evidence to prove a causal link between them. There is better evidence to support the relationship between periodontal disease and stroke. Can a patient’s risk of heart disease and stroke be reduced by treating periodontal disease and improving oral health? The results are not conclusive, however current research seems to trend in favor of the conclusion that improvement of oral health decreases the risk of atherosclerotic disease.
Prevention and Management
For individuals with a family history of heart attack and stroke, it would be prudent to maintain excellent oral hygiene. Regular oral exams and thorough oral care practices, including brushing, flossing, and using an antiseptic mouthwash, are essential in reducing the risk of periodontal disease.
During exams and recall visits to our office, our team will regularly recommend yearly check-ups with the patient’s physician to monitor cardiovascular health. We also take a blood pressure reading during our recall exams. Consistently monitoring can reduce the risk of heart attack and stroke. Regular dental check-ups and cleanings are vital in preventing periodontal disease and tooth loss. Dentists can closely monitor the oral health of patients and help prevent systemic disease from occurring.
Hormone Imbalance and Periodontal Disease

Hormone Imbalance and Oral Health
Hormonal fluctuations, particularly in women, play a pivotal role in influencing the health of the gums and teeth. These hormonal imbalances can significantly impact oral health, and elevate the risk of developing gum disease. Hormone-related shifts can lead to an increased sensitivity in gum tissues and a greater propensity for inflammation.
Prevention and Management
For individuals experiencing hormone imbalances, maintaining good oral hygiene is of paramount importance. Regular and thorough oral care practices, including brushing, flossing, and using an antiseptic mouthwash, are essential in reducing the risk of gum disease associated with hormonal fluctuations.
Pregnant women, who often experience significant hormonal changes, should pay special attention to their oral health. Expectant mothers should consult their dentist to guide their oral health during this critical time. Dental professionals can provide tailored advice and recommendations to address the unique needs of pregnant women and minimize the risk of dental issues.
Menopausal women dealing with hormonal changes can explore hormone replacement therapy (HRT) options to help mitigate the impact of hormonal fluctuations on their oral health. HRT can assist in managing the oral health challenges that may arise during this life phase.
A recent article from the Journal of Periodontal & Implant Science concluded that postmenopausal women had a significantly greater risk of periodontal disease than non-menopausal women. Additionally, the use of HRT in postmenopausal women could reduce the incidence of periodontal disease.
Nevertheless, it is crucial for women to discuss the potential risks and benefits of HRT with their healthcare providers to make informed decisions regarding its usage.
Conclusion
Understanding the connection between these medical conditions and periodontal disease is important not only for improved oral health but also improved systemic health.
Proper prevention and management can help individuals with these conditions maintain their oral health and overall quality of life. By addressing these concerns early and working closely with healthcare professionals, patients can reduce the risk of periodontal disease and associated tooth loss.
At Geach Dental in Downtown Los Angeles and Laguna Niguel, Orange County our team has extensive experience in dealing with dental issues related to these conditions. If you are concerned about potential tooth loss, we encourage you to contact Geach Dental at (213) 622 3339, or click here to schedule a consultation. You deserve to face the world with a healthy, radiant smile!
ABOUT THE AUTHOR: Meet Dr. Adam Geach, distinguished prosthodontics specialist and owner of Geach Dental. His dental education includes Harvard School of Dental Medicine and the University of Connecticut, where he earned a D.M.D. and an M.D.Sc. in Prosthodontics, respectively. Dr. Geach holds Diplomate status with the American Board of Prosthodontics, underscoring his exceptional expertise in dental care.
At his clinics in Los Angeles and Laguna Niguel, Dr. Geach offers a wide range of services, from cosmetic treatments to full-mouth reconstructions, all delivered with a focus on personalized patient care.Take the first step toward your ideal smile and improved oral health by clicking here.
Further Reading:
Vu GT, et al. Tooth loss and uncontrolled diabetes among US adults. The Journal of the American Dental Association 2022; 153(6):542-551.
https://www.sciencedirect.com/science/article/abs/pii/S0002817721007145
Park KY, et al. Association of periodontitis with menopause and hormone replacement therapy: A hospital cohort study using a common data model. Journal of Periodontal & Implant Science 2023; 53(3):184–193. https://doi.org/10.5051/jpis.2202480124
Kane S. The effects of oral health on systemic health. Academy of General Dentistry 2017; 411:30-34.