A radiant smile is not only a symbol of beauty but also a reflection of one’s self-confidence and overall well-being. Full-mouth reconstructions, a highly specialized treatment within prosthodontics, have gained recognition for their ability to restore and or replace both the aesthetics and function of a person’s teeth .
Full-mouth reconstructions go beyond cosmetic enhancement. They are designed to give individuals a renewed sense of self-assurance and the ability to enjoy life fully. This transformational journey begins with a detailed assessment and meticulous planning, as every case is unique, presenting its challenges and opportunities.
In this article, we’ll walk you through the journey of a patient who, like many others, was confronted with the harsh reality of decayed and broken teeth, see pictures below. The impact of her dental condition went beyond mere physical discomfort. It extended to her self-esteem, her social interactions, and even her dietary choices.
This case, although challenging, serves as a testament to the power of modern prosthodontics to restore not only the aesthetics of one’s smile but also the functionality that is crucial for a better quality-of-life. Because all of the teeth were non-restorable, the plan was to replace the teeth with dental implant bridges (also called All-on-4).
Initial Assessment and Planning
When embarking on a full-mouth reconstruction, meticulous planning is the cornerstone of a successful transformation. The significance of this phase cannot be overstated, as it lays the groundwork for the entire journey.
Making Impressions:
- Impressions are the first essential step in designing the new set of teeth. They serve as the building blocks in which the entire procedure is constructed.
- Impressions are now made digitally to capture the unique characteristics of the patient’s oral structures. A digital 3D model is created to begin planning the reconstruction.
Evaluation of the Face and Smile Line:
- Careful evaluation of the patient’s face and smile line is imperative. This evaluation goes beyond the confines of the oral cavity and extends to the patient’s entire facial structure.
- Each individual’s smile line is unique, and the new teeth must harmonize with the smile to achieve both aesthetic and functional success.
This initial phase ensures that the treatment plan is tailor-made to suit the patient’s specific needs. It is here that the foundation is laid for a smile that not only looks beautiful but also functions optimally, bringing a renewed sense of confidence and comfort to the patient’s life.
Bone Assessment and Implant Placement
Assessing the underlying bone structure and the strategic placement of dental implants play pivotal roles. This phase is crucial for ensuring long-term success and functionality.
Role of Bone Assessment:
- Before any treatment can proceed, a thorough assessment of the jawbone is essential. The height and width of the bone help to determine the proper position of the dental implants.
- This assessment guides the treatment planning, helping prosthodontists make informed decisions about how the teeth will be replaced.
Utilizing X-rays and CT Scans:
- To conduct a comprehensive evaluation of the jawbone, CT scans are utilized. These 3-dimensional images allow for precise measurements of the bone and to visualize vital structures.
- CT scans enable the prosthodontist to visualize the volume of bone and make informed decisions about the position of the dental implants. The image below shows the locations of where implants will be placed in the upper jaw.
Dental Implant Placement:
- Dental implant placement is a critical step in the restoration process. It is important to create a solid foundation for the final restorations.
- Implants serve as the foundation for the prosthetic teeth. They are carefully positioned using a surgical guide based on the information shown above. The goal is to maximize the spacing of the implants so that the biting forces on the implant bridges can be well distributed.
The careful combination of bone assessment, imaging technology, and precise dental implant placement ensures that the smile makeover not only appears visually stunning but also functions seamlessly, allowing the patient to enjoy a more fulfilling life.
Prosthetic Restoration
Immediately following the placement of dental implants, the treatment enters the phase of prosthetic restoration. This phase is where the patient’s vision of a complete, beautiful, and functional smile takes shape.
Crucial Post-Implant Placement Phase
- The post-implant placement phase is a pivotal step in the reconstruction process. After dental implant surgery, a period of healing and osseointegration is crucial.
- Osseointegration refers to the process where the bone fuses with the implant, ensuring its stability and long-term success.
- Immediately after implant placement, temporary implant bridges are adjusted and inserted into the implants to provide immediate function and aesthetics. These temporary, full-arch bridges actually help to secure the implants during the healing phase.
The Healing Phase is Crucial
- The healing period, typically lasting around three months, allows the dental implants to fully integrate with the jawbone.
- This phase is fundamental to the overall success of the prosthetic restoration, as it provides the necessary stability for the final prosthetic implant bridges.
Crafting the Final Upper and Lower Implant Bridges
Once the healing period is complete, the prosthodontist proceeds to design and fabricate the final implant bridges. See final pictures below.
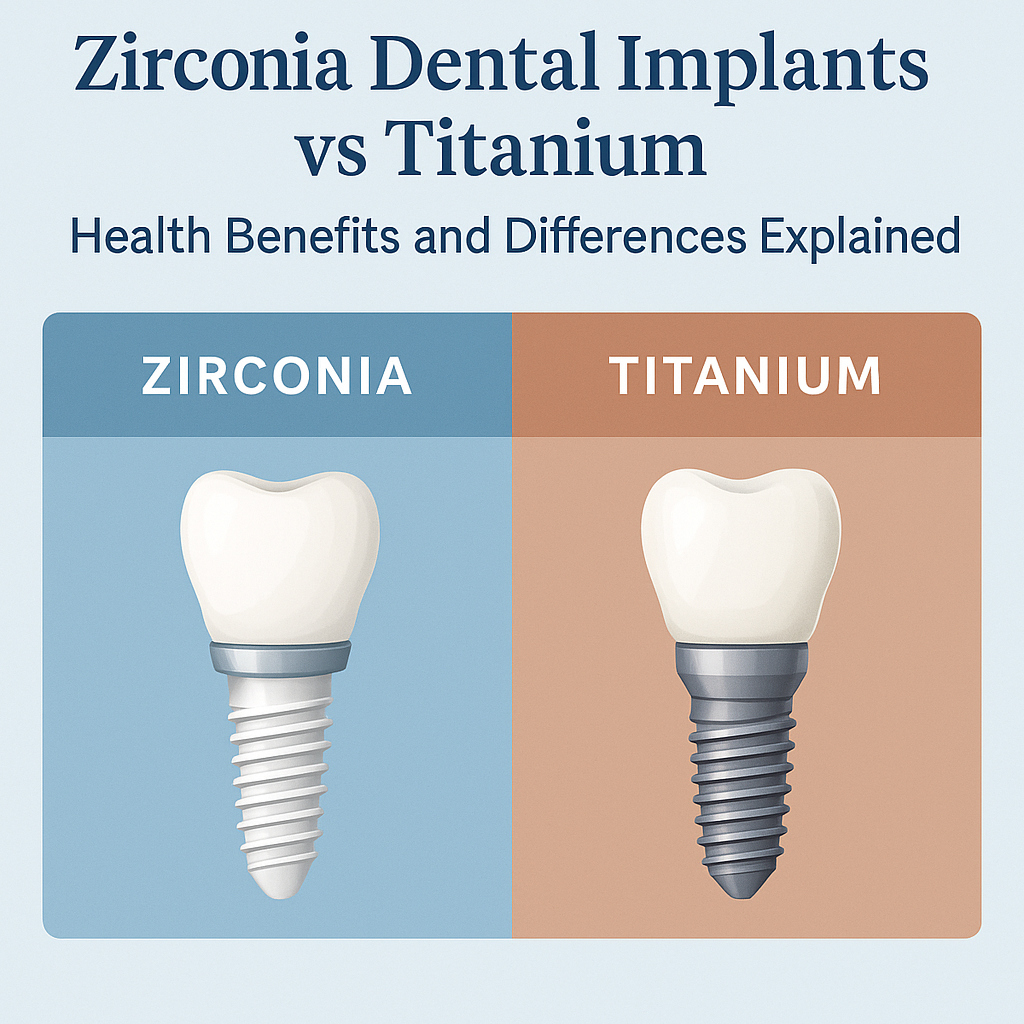
- For the upper teeth, a carefully designed zirconia implant bridge was milled to fit precisely into the 6 implants. Artistic characterization like surface texture, shade and shape are added to create a lifelike appearance.
- In the lower jaw, a similar permanent implant bridge was carefully crafted to fit seamlessly onto the four dental implants. This bridge is designed to occlude precisely into the upper bridge to restore functionality.
This final prosthetic phase brings the full-mouth reconstruction full circle, giving life to the patient’s vision of a new, beautiful smile that not only looks natural but functions optimally. It’s the culmination of a comprehensive process that has the power to renew self-confidence, comfort, and overall quality-of-life.
Transform Your Smile, Transform Your Life!
The remarkable transformation achieved through a full-mouth reconstruction is a testament to the power of a captivating and confident smile. It’s not just a cosmetic enhancement; it’s a life-changing experience that seamlessly blends aesthetics and functionality.
The impact of a full-mouth reconstruction is profound, reaching beyond the dental chair to touch the core of an individual’s self-esteem, social interactions, and dietary choices. The patient, who initially faced the challenges of broken teeth, emerged from this process with a renewed sense of self-confidence, comfort, and overall well-being.
For those considering a similar path to improved dental health and confidence, understanding the process of a full-mouth reconstruction is paramount. With the guidance and expertise of prosthodontic specialists, you can embark on a transformative journey that enhances your aesthetics and boosts your confidence for years to come.
If you’re wondering whether it’s time for your full-mouth reconstruction, the advanced knowledge and specialized expertise of our prosthodontic team at Geach Dental are at your service. With locations in Downtown Los Angeles and Laguna Niguel, Orange County, our dedicated team ensures that each patient receives exceptional care in a comfortable and supportive environment.
We are committed to empowering our patients with a thorough understanding of their upcoming procedures, ensuring you are well informed about the associated risks and rewards. Our priority is your comfort and well-being throughout the process.
To take the first step towards your radiant smile, simply call us today at (213) 622-3339 or click here to schedule a consultation. Your dental wellness is our top priority, and we are ready to support you on your journey to a healthier, more confident smile.
ABOUT THE AUTHOR: Meet Dr. Adam Geach, distinguished prosthodontics specialist and owner of Geach Dental. His dental education includes Harvard School of Dental Medicine and the University of Connecticut, where he earned a D.M.D. and an M.D.Sc. in Prosthodontics, respectively. Dr. Geach holds Diplomate status with the American Board of Prosthodontics, underscoring his exceptional expertise in dental care.
At his clinics in Los Angeles and Laguna Niguel, Dr. Geach offers a wide range of services, from cosmetic treatments to full-mouth reconstructions, all delivered with a focus on personalized patient care.Take the first step toward your ideal smile and improved oral health by clicking here.