In modern dentistry, dental implants have revolutionized tooth replacement, offering functional reliability and enhanced aesthetics. This article assesses the success rates of dental implants, providing crucial insights for patients. How successful is dental implant treatment?
We’ll explore this question to shed light on the potential transformation that dental implants offer. If you’re a patient seeking answers, this exploration of dental implant success promises invaluable insights.

What Are Dental Implants?
Dental implants are cutting-edge prosthetic devices that have redefined the landscape of tooth replacement in modern dentistry. They serve as a reliable, long-lasting solution for individuals with missing teeth, restoring not only their smiles but also their oral function.
The three primary components of a dental implant are:
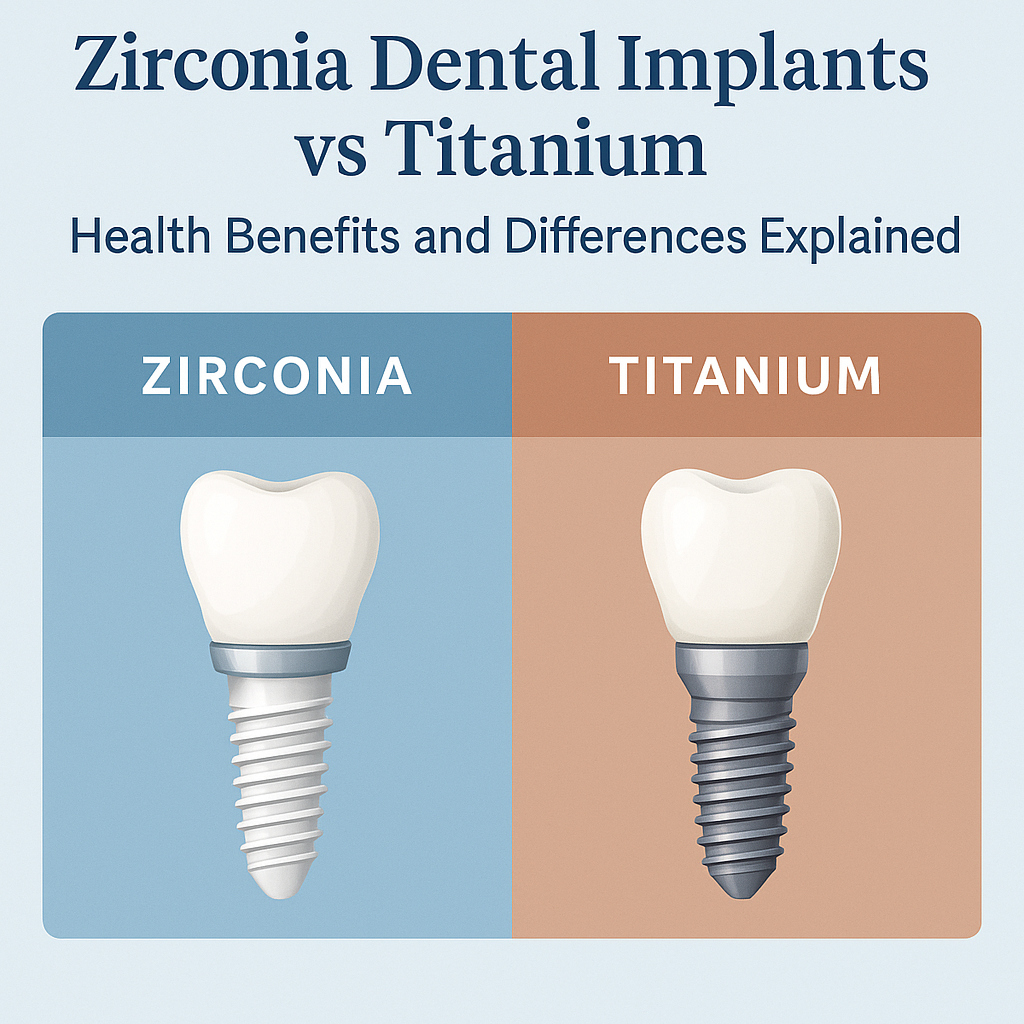
- The Implant: This is the anchor, typically made of biocompatible materials like titanium, which is surgically placed into the jawbone. The implant functions as a root replacement, providing a sturdy foundation for the restoration.
- The Abutment: Once the implant has integrated with the jawbone, an abutment is attached. The abutment connects the implant to the prosthetic crown and plays a crucial role in stability.
- The Prosthetic Crown: This is the visible part of the dental implant and is custom-designed to match the patient’s natural teeth in color, shape, and function. It is securely attached to the abutment and functions like a natural tooth.

The Advantages of Dental Implants Over Other Tooth Replacement Options
The benefits of dental implants include:
- Durability: Dental implants are designed to last, often for a lifetime, making them a long-term investment in oral health.
- Natural Aesthetics: Implants provide a remarkably realistic appearance, ensuring a seamless blend with existing teeth.
- Improved Function: Dental implants restore full chewing function, allowing you to eat, speak, and smile with confidence.
- Preservation of Bone: Unlike some alternatives, dental implants stimulate the jawbone, preventing bone loss and maintaining bone structure.
- Convenience: Implants do not require special maintenance and do not affect neighboring teeth, as is often the case with dental bridges.
In summary, dental implants are innovative devices that serve as a reliable and long-lasting solution for missing teeth. They consist of an implant, abutment, and prosthetic crown, providing patients numerous advantages, including natural aesthetics, restoration of function, and overall convenience. These qualities contribute to their popularity with many patients.

The Success Criteria of Dental Implants
The success of dental implant treatment hinges on critical factors that are pivotal in ensuring favorable outcomes for patients. Understanding these factors is essential for both patients and prosthodontists embarking on the journey of using dental implants for tooth replacement.
Critical Factors for Success
In conclusion, the success of dental implant treatment is determined by a careful selection of patients, their overall health, and the skill of the prosthodontist. These key factors, combined with diligent aftercare and maintenance, ensure the best chances of success for patients seeking to restore their smiles with dental implants.
Success Rates of Dental Implants
Understanding the success rates of dental implant treatment is paramount for patients considering this transformative dental solution. This section provides insights into the factors influencing these rates and offers different scenarios for successful implantation.
Success Rates and Research Findings
Studies consistently demonstrate that dental implant treatment boasts an impressive success rate, typically exceeding 95%. These rates are influenced by various factors, including the overall health of the patient, the site of implantation, and the prosthodontist’s expertise.
Immediate vs. Delayed Loading
- Immediate Loading: In some cases, implants can be loaded with a crown shortly after placement. Success rates for immediate loading are generally high, with careful case selection, patient health, and precision in implant placement being critical.
- Delayed Loading: Delayed loading involves a healing period before attaching the prosthetic crown to the implant. This approach often yields equally high success rates, with the added benefit of allowing the implant to integrate fully with the bone.
Success Rates for Different Scenarios:
- Single Implants: Dental implants used to replace single missing teeth enjoy exceptional success rates, often surpassing 98%. This is due to the simplicity of the procedure and the reduced impact on surrounding teeth.
- Multiple Implants: Success rates for multiple implants used to replace several missing teeth remain consistently high, typically exceeding 95%. Thorough case assessment and meticulous planning are crucial.
- Full-Mouth Restorations: While full-mouth restorations involving numerous implants are more complex, they can still achieve success rates of 90% or higher with proper patient selection and expert care.
It is important to note that success rates can vary based on individual circumstances, emphasizing the importance of working closely with a skilled prosthodontist to maximize the potential for a successful dental implant treatment.

Factors Influencing the Success of Dental Implants
An interplay of patient-related factors, surgical techniques, and maintenance influences the success of dental implant treatment. Understanding these aspects is essential for patients and practitioners alike.
- Overall Health: Patient health is a critical factor. Medical conditions like uncontrolled diabetes and autoimmune disorders can affect the healing process. Maintaining good general health through lifestyle and medical management is critical.
- Bone Quality: The density and quality of the jawbone at the implant site are paramount. A strong and healthy jawbone ensures a solid foundation for the implant. Bone grafting may be necessary in cases of poor bone quality.
- Smoking Habits: Smoking has a detrimental impact on implant success. It can impede healing, increase the risk of infection, and lead to implant failure. Patients are advised to quit smoking or avoid it during the implant process.
In conclusion, the success of dental implant treatment is influenced by patient-related factors such as overall health, bone quality, and smoking habits. Additionally, the surgical technique and choice of implant system are significant determinants. Proper maintenance, follow-up care, and a commitment to oral hygiene are essential for ensuring long-term implant success.
Potential Complications and How to Mitigate Them
While dental implant treatment is highly successful, it’s essential to be aware of potential complications and how to address them. Here, we’ll outline common issues and strategies for prevention and management.
Potential Complications
- Infection: Infections can occur during or after the implant procedure. Proper sterilization, antibiotics, and careful post-operative care can mitigate this risk.
- Implant Failure: Implant failure, where the implant does not integrate with the bone, is rare but possible. It may result from factors like poor bone quality or incorrect implant placement.
- Peri-Implantitis: This inflammatory condition affects the tissues surrounding the implant, leading to bone loss and implant instability if left untreated.
Preventive Measures and Treatment
- Infection Prevention: Ensure your prosthodontist follows strict sterilization protocols. Post-operatively, take prescribed antibiotics and follow hygiene instructions diligently.
- Implant Failure Mitigation: To prevent implant failure, it’s crucial to select a qualified prosthodontist who uses high-quality implant systems. Bone grafting may be an option for patients with poor bone quality.
- Managing Peri-Implantitis: Regular follow-up appointments are crucial for early detection. In the case of peri-implantitis, treatment may involve professional cleaning, antibiotics, and, in severe cases, surgical intervention.
Importance of Regular Follow-Up Appointments
Regular follow-up appointments with your prosthodontist are vital for several reasons:
- They allow for the early detection of complications, ensuring prompt intervention.
- Routine check-ups help maintain proper oral hygiene and prevent peri-implantitis.
- Proactive monitoring safeguards the long-term success and stability of your dental implants.
In short, while dental implant treatment is highly successful, complications like infection, implant failure, and peri-implantitis can occur. Preventive measures and vigilant follow-up appointments with your prosthodontist are crucial for addressing these issues and maintaining the long-term health of your dental implants.
Summary
Dental implants can transform your oral health and leave you with a more functional and confident smile. Understanding the process of dental implant treatment and how to maintain your enhanced smile can help you make an informed decision about this transformative procedure that will improve your dental well-being and self-assurance for years.
If you’re considering dental implants as a solution for missing teeth, the advanced knowledge and specialized expertise of our prosthodontic team at Geach Dental, located in Downtown Los Angeles and Laguna Niguel, Orange County, are here to help ensure you achieve the attractive and confident look you deserve.
To take the first step toward a healthier and more confident smile, call us today at (213) 810 3368 or click here to schedule a consultation. Your dental wellness is our top priority, and your journey toward a healthier and more beautiful smile starts here!
ABOUT THE AUTHOR: Meet Dr. Adam Geach, distinguished prosthodontics specialist and owner of Geach Dental. His dental education took in Harvard School of Dental Medicine and the University of Connecticut, where he earned a D.M.D. and an M.D.Sc. in Prosthodontics, respectively. Dr. Geach holds Diplomate status with the American Board of Prosthodontics, underscoring his exceptional expertise in dental care.
At his clinics in Los Angeles and Laguna Niguel, Dr. Geach offers a wide range of services, from cosmetic treatments to full-mouth reconstructions, all delivered with a focus on personalized patient care.Take the first step toward your ideal smile and improved oral health by clicking here.