Dental Tourism, a prominent subset of Medical Tourism, has gained significant popularity in recent years, drawing patients from various parts of the world, including the United States.
While many individuals opt for Dental Tourism to access affordable dental care, one destination that stands out for Americans, particularly those residing in Southern California, is Mexico. The proximity and cost-effectiveness of dental treatments in Mexico make it an attractive choice for those seeking oral healthcare solutions.
Patients seeking dental treatments in Mexico often hope to achieve substantial cost savings compared to what they might pay for similar procedures in the United States. However, behind the allure of affordability, there lies a series of hidden risks and complications.
In this article, we will focus on Dental Tourism, considering Mexico as a prime destination, and the hidden pitfalls that patients may encounter. While some individuals may indeed experience successful outcomes with dental implants, bridges, crowns, and dentures in Mexico, I have seen many patients experience various problems and complications.
Our goal is to provide you with an informative and comprehensive guide, enabling you to make informed decisions when it comes to your oral health. Drawing from real-life patient experiences and expert insights, we will explore the nuances of dental tourism, the promise it holds, and the caution that one must exercise when venturing into this world of affordable dentistry abroad.

Understanding Medical and Dental Tourism
What is medical and dental tourism?
Medical and Dental Tourism involves traveling to other countries for medical or dental procedures and seeking cost-effective alternatives to the treatments available in one’s home country. The potential for significant savings without compromising the quality of care they receive drives patients to pursue this solution.
Reasons for choosing medical and dental tourism
The primary motivation behind medical and dental tourism is cost savings. In many cases, medical and dental procedures in certain countries can cost a fraction of what they would in the patient’s home country. This financial advantage makes it an appealing choice, particularly for those without comprehensive insurance coverage or facing long treatment waiting times.
Common destinations for medical and dental tourism
While medical and dental tourism can take patients to various countries worldwide, Mexico is a preferred destination for Americans, especially those residing in Southern California. Proximity, lower costs, and cultural familiarity make it a top choice for dental procedures.
Types of medical and dental procedures sought after
A wide range of medical and dental procedures is sought after in the field of medical and dental tourism. Dental treatments, such as implants, bridges, crowns, and dentures, are among the most commonly sought services due to their high costs in some countries. Additionally, cosmetic surgeries, elective surgeries, and specialized medical treatments draw patients to destinations worldwide.

The Allure of Cost Savings
The attraction of cost savings in medical and dental tourism
One of the primary driving factors behind the popularity of medical and dental tourism is the significant cost savings it offers. Patients often find that the cost of medical and dental procedures in their home countries can be prohibitively high. By opting for treatment abroad, they can access quality healthcare services at a fraction of the cost, which makes these treatments more affordable and accessible.
Comparative cost of treatments at home vs. abroad
To put the allure of cost savings into perspective, consider this: a dental implant procedure in the United States may cost thousands of dollars, whereas the same procedure in a destination like Mexico can be considerably cheaper. This substantial price difference is a compelling reason for many individuals to venture into the world of medical and dental tourism. Keep in mind that a dental tourist may be abroad for about 15 days, with an average of 8 days for a single procedure. The cost of travel and hotel must be factored into the overall cost (1).
Factors contributing to lower costs in foreign countries
Several factors contribute to the lower costs of medical and dental treatments in foreign countries. These include:
- Lower labor and operating costs, reduced administrative expenses, and a lower overall cost of living. Additionally, currency exchange rates can further amplify the cost-effectiveness for patients from countries with stronger currencies.
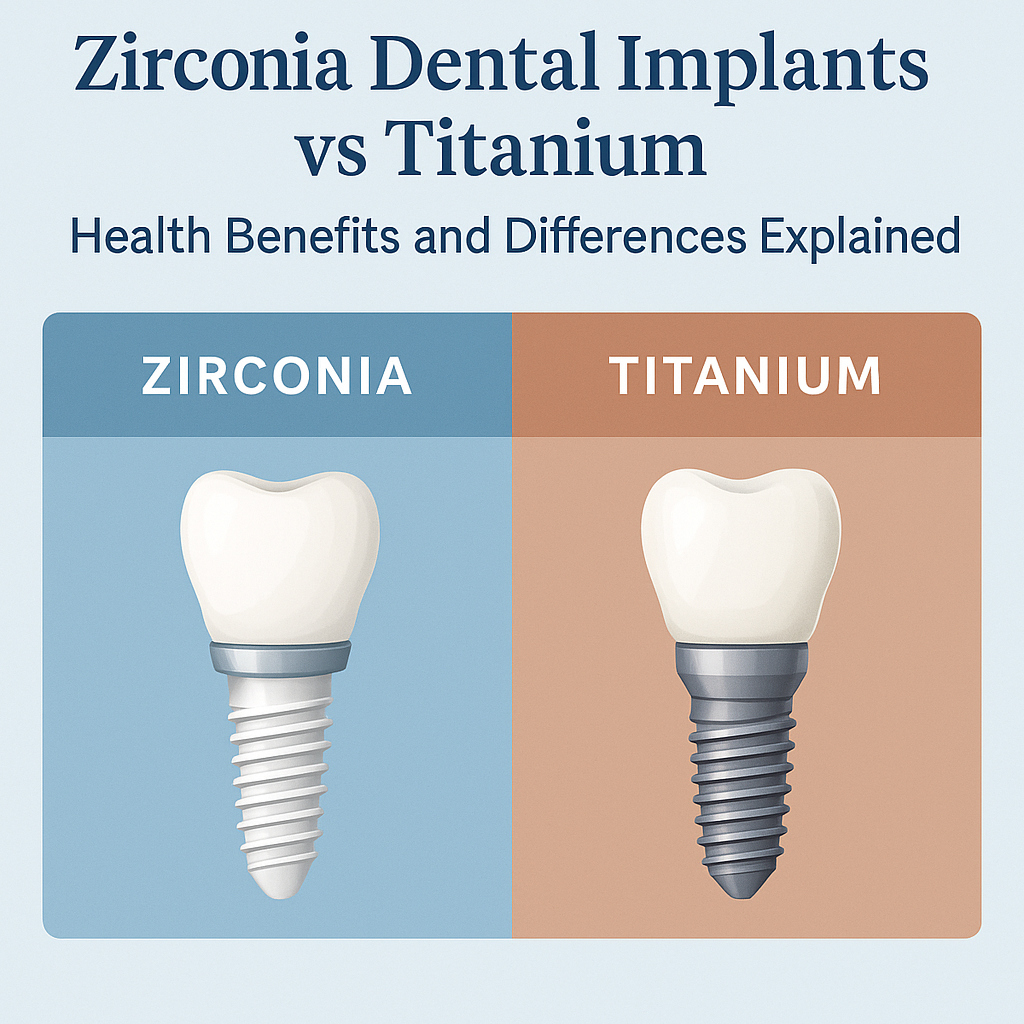
- Use of less expensive dental materials, dental implants, dental implant components and laboratories for fabrication of the dental restorations. Understanding the quality of the dental materials and components used is critical. Use of lower quality materials can lead to complications such as implant failure and fracture of the restorations.
Understanding the economic drivers behind cost savings is essential for patients considering medical and dental tourism. While affordability is undoubtedly attractive, it’s crucial to recognize that these savings can come with hidden risks and potential complications, as we will explore in the subsequent sections.
Hidden Risks and Complications
Quality of Care
- Variability in healthcare standards: Medical and dental tourism often involves navigating a landscape of varying healthcare standards. While some facilities may uphold high-quality care, others may not meet the same rigorous standards. The lack of uniformity can lead to uncertainty regarding the quality of care received.
- Regulatory and accreditation issues: Different countries have their own regulatory bodies and accreditation standards for healthcare facilities. Some destinations may not have stringent oversight or rigorous accreditation processes, potentially exposing patients to facilities that do not meet internationally recognized quality benchmarks.
- Post-operative complications: Patients need to understand that there are post-operative risks involved in air travel. For example, it is recommended to wait 2 weeks following sinus lifts or extensive bone grafting procedures to avoid sinus problems (1).
- Lack of aftercare and follow-up: Once the procedure is completed abroad, patients may face challenges securing necessary aftercare or follow-up care in their home country. This gap in continuity of care can lead to complications or difficulties in addressing post-treatment issues.
- Language barriers and communication challenges: Effective communication between patients and healthcare providers is paramount. Language barriers can hinder the exchange of critical information, leading to misunderstandings and miscommunication that may impact the patient’s treatment and overall experience.
Infection Control and Safety
- Variances in hygiene and sterilization practices: Hygiene and sterilization standards can differ between countries and facilities. Inconsistent practices can pose risks of infection or contamination, potentially jeopardizing patient safety during medical and dental procedures.
- Exposure to infectious diseases: Patients traveling for medical and dental tourism may encounter regions with a higher prevalence of infectious diseases. This exposure can increase the risk of contracting diseases that may not be as prevalent in their home country.
- Risks associated with unregulated facilities: Some medical and dental facilities in foreign countries may operate with limited regulation and oversight. This lack of regulation can result in substandard safety protocols, increasing the potential for complications.
- Handling of medical and dental waste: Proper disposal of medical and dental waste is a critical component of healthcare safety. Facilities in specific destinations may not adhere to rigorous waste management standards, posing environmental and health risks.
Legal and Ethical Concerns
- Understanding legal recourse and liability: Patients who experience complications or adverse outcomes may find it challenging to pursue legal recourse in a foreign country. Different legal systems and limited familiarity with local laws can complicate efforts to seek compensation or resolution.
- Challenges in seeking compensation or resolution: The process of seeking compensation or resolution for medical or dental complications can be arduous, time-consuming, and costly. Patients may face difficulties holding foreign healthcare providers accountable for negligence or malpractice.
- Ethical dilemmas in foreign medical and dental practices: Ethical standards in healthcare may vary across countries. Patients may encounter situations where the ethical considerations of a foreign medical or dental practice differ from what they are accustomed to in their home country.
These hidden risks and complications underscore the need for patients to carefully consider the potential downsides of medical and dental tourism before embarking on such a journey.
Minimizing Risks and Making Informed Choices
Tips for researching healthcare providers and facilities
- Conduct thorough research: Before embarking on a medical or dental tourism journey, research potential healthcare providers and facilities. Read reviews, check their credentials, and assess their track record in providing the specific procedure you need.
- Request patient testimonials: See testimonials from previous patients who have undergone similar procedures at the facility you are considering. Hearing about their experiences can provide valuable insights into the quality of care and outcomes.
- Verify credentials: Ensure that healthcare providers are licensed and are trained in accredited dental programs. Check for board certification if you are being treated by a dental specialist. Research the regulatory bodies and standards applicable in the destination country to confirm their legitimacy.
- Consult your local healthcare professional: Talk to your primary care physician or dentist about your decision to pursue treatment abroad. They can offer guidance, provide recommendations, and assess whether you are a suitable candidate for medical or dental tourism.
Pre-travel preparations and questions to ask
- Obtain comprehensive medical records: Request your medical or dental records from your home healthcare provider to share with your chosen facility abroad. These records are essential for accurate diagnosis and treatment planning.
- Communicate your medical history: Be transparent about your medical history, including allergies, chronic conditions, medications, and prior surgeries. This information is crucial for ensuring your safety during treatment.
- Ask about treatment plans and costs: Request a detailed treatment plan, including all associated costs, so you have a clear understanding of what to expect. Inquire about potential additional charges or hidden fees.
- Clarify follow-up and aftercare: Discuss the post-treatment care and follow-up procedures. Ensure that you are aware of what to do if complications arise and how to seek assistance or guidance.
Importance of seeking second opinions
- Consult multiple healthcare professionals: Seek second opinions from different healthcare providers in your home country. This process can help you verify the diagnosis, treatment recommendations, and costs associated with your dental procedure.
- Compare recommendations: By obtaining multiple opinions, you can compare the suggested treatment options and make more informed decisions regarding your dental healthcare.
- Ensure alignment with your preferences: Second opinions can also help you find a dental healthcare provider whose approach aligns with your priorities and comfort level.
By following these guidelines and taking a proactive approach, you can minimize the risks associated with medical and dental tourism while ensuring you make informed choices for your dental healthcare abroad.
Conclusion
Throughout this article, we’ve explored the often-overlooked challenges associated with medical and dental tourism, shedding light on the hidden risks and complications patients may encounter when seeking healthcare abroad. As we conclude, it’s vital to make informed decisions and prioritize safety over cost.
While the prospect of cost savings is a significant draw for medical and dental tourism, patient safety and quality of care should always remain paramount. The value of healthcare goes beyond its financial aspects; it encompasses the assurance of receiving high-quality care and ensuring your well-being throughout the entire healthcare journey.
For you’re considering dental treatment abroad, the advanced knowledge and specialized expertise of our prosthodontic team at Geach Dental, conveniently located in Downtown Los Angeles and Laguna Niguel, Orange County, are a safe alternative and will ensure you get the safe treatment and outcome you deserve.
We’ll go the extra mile to make sure you understand your upcoming procedure as well as all of its risks and rewards. And we’ll spend as much time as you need talking to you to make sure we’re both on the same page and you are 100% comfortable with the plan we agree on.
To take the first step towards a radiant smile, simply call us today at (213) 622-3339 or click here to schedule a consultation. Your dental wellness is our top priority and your journey towards a healthier smile starts here!
In conclusion, medical and dental tourism can offer opportunities for cost saving – once flights and hotel costs are removed from the equation. However, it is crucial to approach this decision with caution and thorough research. By making informed choices, you can strike a balance between affordability and safety, ensuring that your healthcare experience is one of confidence and peace of mind. Your health and well-being deserve nothing less.
References
- Felkai P, et al. Dental tourism and the risk of barotrauma and barodontalgia. British Dental Journal. 2023; 234: 115-117.
ABOUT THE AUTHOR: Meet Dr. Adam Geach, distinguished prosthodontics specialist and owner of Geach Dental. His dental education includes Harvard School of Dental Medicine and the University of Connecticut, where he earned a D.M.D. and an M.D.Sc. in Prosthodontics, respectively. Dr. Geach holds Diplomate status with the American Board of Prosthodontics, underscoring his exceptional expertise in dental care.
At his clinics in Los Angeles and Laguna Niguel, Dr. Geach offers a wide range of services, from cosmetic treatments to full-mouth reconstructions, all delivered with a focus on personalized patient care. Take the first step toward your ideal smile and improved oral health by clicking here.