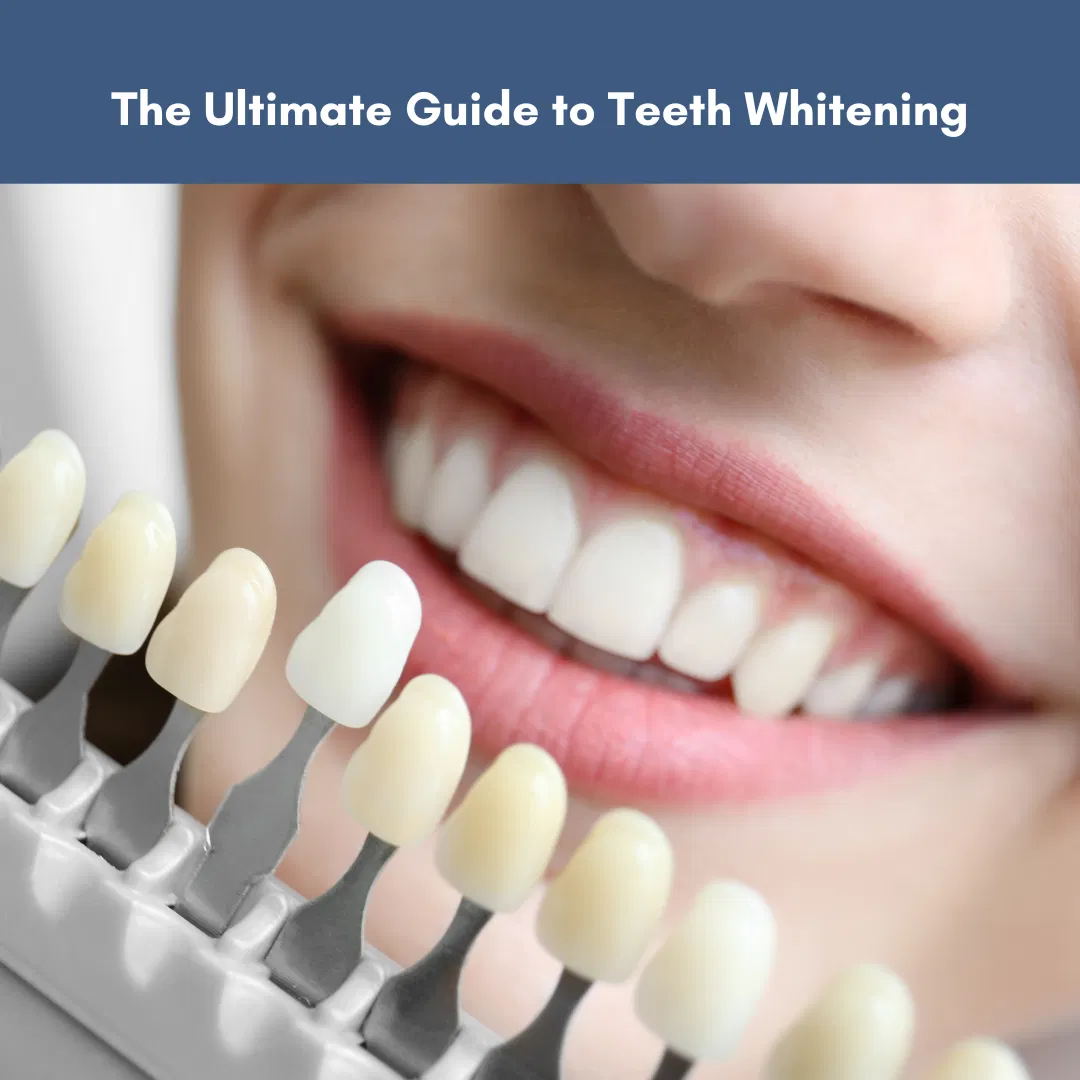
Teeth whitening is one of the most sought-after cosmetic dentistry procedures, promising us a brighter, more confident smile. In the quest for whiter teeth, many people turn to over-the-counter treatments for a convenient solution. However, the allure of these readily available options often masks their limitations and potential drawbacks.
Over-the-counter products may lack the potency to address stains effectively compared to more customized solutions. The one-size-fits-all approach can lead to uneven results, causing some teeth to whiten more than others. Additionally, these products may not account for individual oral health conditions, potentially exacerbating existing issues such as tooth sensitivity or gum irritation.
At Geach Dental, we aim to equip you with the knowledge to make informed decisions, steer clear of the pitfalls of generic solutions, and guide you toward a brighter, healthier smile. In this comprehensive guide, we will explain everything you need to know about the intricacies of teeth whitening.
Understanding Teeth Discoloration
Teeth are composed of two main components, enamel and dentin. Enamel is the outer part of the tooth and is made of hydroxyapatite. Pure hydroxyapatite is colorless/white and natural enamel has a white color with some translucency. Dentin is the inner part of the tooth and is composed of 70% hydroxyapatite with proteins and water representing the other 30%. Dentin naturally has a more yellowish hue. Over time, the youthful brightness of our smile can fade. With continuous chemical and mechanical wear of enamel over time, the enamel becomes thinner and more translucent making the inner dentin more visible, resulting in a darker tooth color. Furthermore, the natural white color of teeth can be compromised due to stains from pigmented foods, wine, tea, coffee, smoking, etc.
Types of Teeth Stains
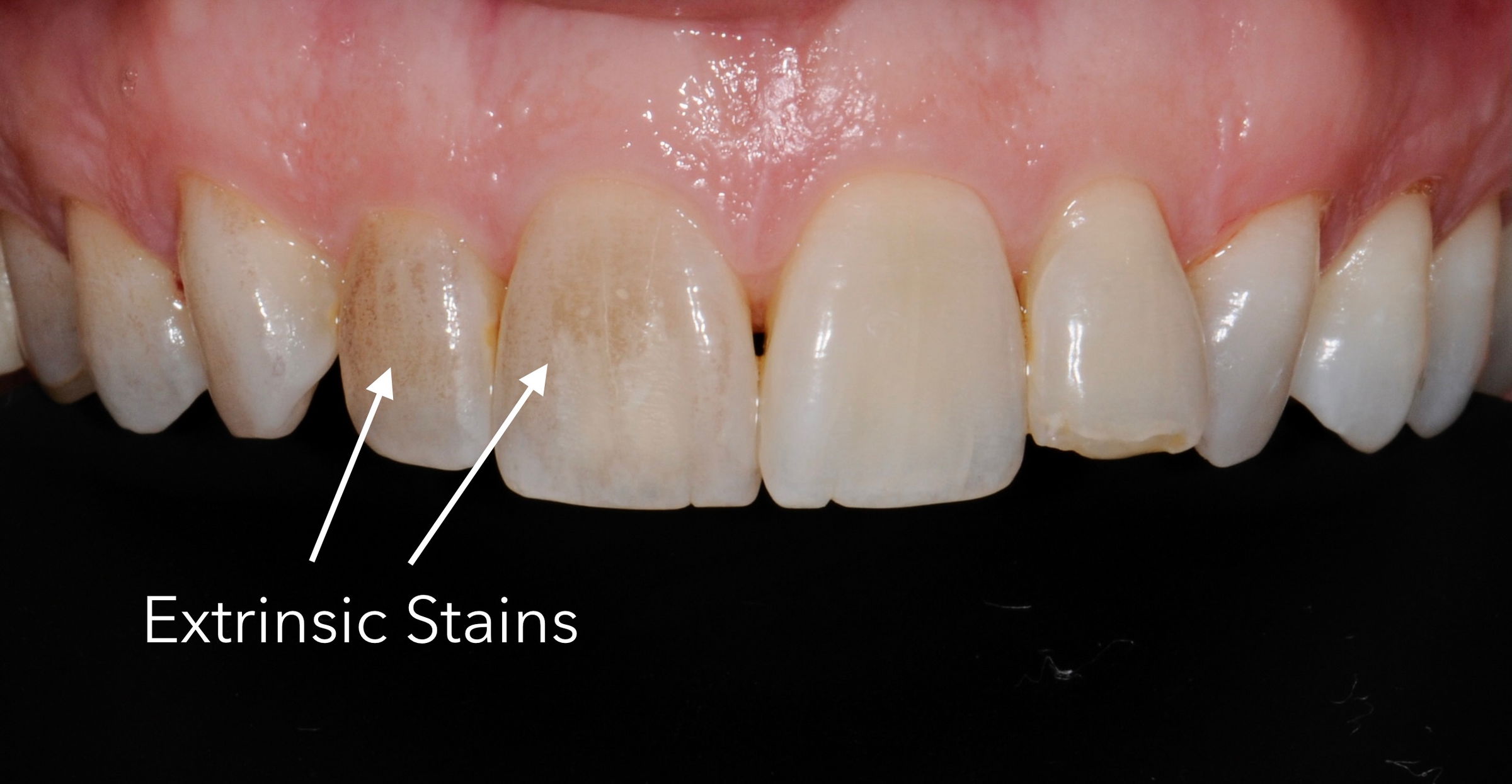
- Extrinsic Stains:
Extrinsic stains present on the outer surface of the tooth – on enamel or exposed dentin. These stains are often caused by organic chromophores such as tannins from pigmented fruits, coffee, tea or red wine. Regular consumption of these foods and beverages or habitual smoking can contribute to the gradual accumulation of extrinsic stains on the tooth surface.
- Intrinsic Stains:
Intrinsic Stains, on the other hand, occur within the tooth structure, affecting the enamel or underlying dentin. These stains may result from factors during tooth formation such as excessive fluoride intake, medications such as tetracycline and metabolic diseases during tooth development. Intrinsic staining can also happen after tooth eruption. Trauma can cause hemorrhage in the tooth leading to discoloration by blood penetrating into the dentin. Certain procedures such as amalgam or root canal fillings can also produce intrinsic stains.

The Most Common Causes of Discoloration
Environmental Factors:
Over time, teeth naturally change color due to environmental influences. Highly acidic beverages erode the surface of the enamel. Thinning of the white enamel leads to more yellowish coloration due the appearance of the underlying dentin. Mechanical grinding of teeth will flatten the enamel on the cusps of teeth also leading to yellowish shades.
Food and Beverages:
Certain foods and beverages contain pigments that can stain teeth over time. Colored fruits, berries, and beverages such as tea, coffee and red wine are common culprits. Regular consumption of these items can contribute to accumulating extrinsic stains on the tooth surface.
Tobacco Use:
Smoking or using tobacco products introduces harmful chemicals to the oral environment, leading to stubborn extrinsic stains. The tar and nicotine in tobacco can discolor teeth, affecting the enamel and underlying dentin.
Medications:
Medications such as tetracycline, can cause intrinsic stains during tooth development. These stains may present as gray or brown discolorations, emphasizing the need for awareness and professional guidance when considering teeth whitening options.
Understanding the diverse nature of teeth stains and their underlying causes is crucial in formulating effective teeth whitening strategies. So, in the following sections, we will explore professional and at-home whitening options, considering individual needs and the nature of discoloration.
In-Office vs. At-Home Teeth Whitening
Options for Professional Teeth Whitening
A smile makeover is a meticulous and personalized process, with each step designed to achieve a stunning and confidence-boosting result. Here’s an in-depth look at the step-by-step process involved in a smile makeover:
In-office Treatments:
In-office teeth whitening procedures administered in the dental office are performed with concentrated solutions of 35% hydrogen peroxide for about 20-30 minutes. These high concentrations of hydrogen peroxide are oxidizing and can harm the soft tissues. In addition, In-office whitening can also cause irritation of the dental pulp in some individuals (1). A heat lamp or blue light is often used to enhance the oxidative action of the peroxide. Based on clinical studies, addition of a blue light has not been proven to enhance the whitening effect or the persistence of the whitening treatment (2). We do not offer in-office treatments in our practice because of the risk of gum irritation and extreme tooth sensitivity.
Custom take-home whitening kits:
Take-home whitening kits use 10-20% carbamide peroxide gel that is applied to the teeth using a patient-specific mouthguard. A 10% carbamide gel has been approved by the American Dental Association for home whitening. The lower concentration of the gel requires multiple applications to achieve visible effects. In our practice, we recommend a 16% carbamide peroxide gel to be applied to the teeth using a custom mouthguard for 1-2 hours per day for 10 days. This combination provides a blend of professional-grade efficacy and the convenience of home application. The lower concentration gel also reduces gum irritation and tooth sensitivity. Some patients have teeth that are very sensitive to the 16% gel and this can be substituted with a 10% gel.
Are Over-The-Counter White Strips a Cost-Effective Alternative?
A common question that is asked in our practice is: Does the use of over-the-counter whitening strips exhibit similar whitening results compared to custom take-home kits?
Manufacturers claim that whitening strips show good whitening results at a lower cost and can be easily found online, in markets and pharmacies. Independent clinical studies show that over-the-counter whitening strips can perform about as well as dentist supervised custom take-home kits for whitening teeth (3).
Benefits of OTC whitening strips:
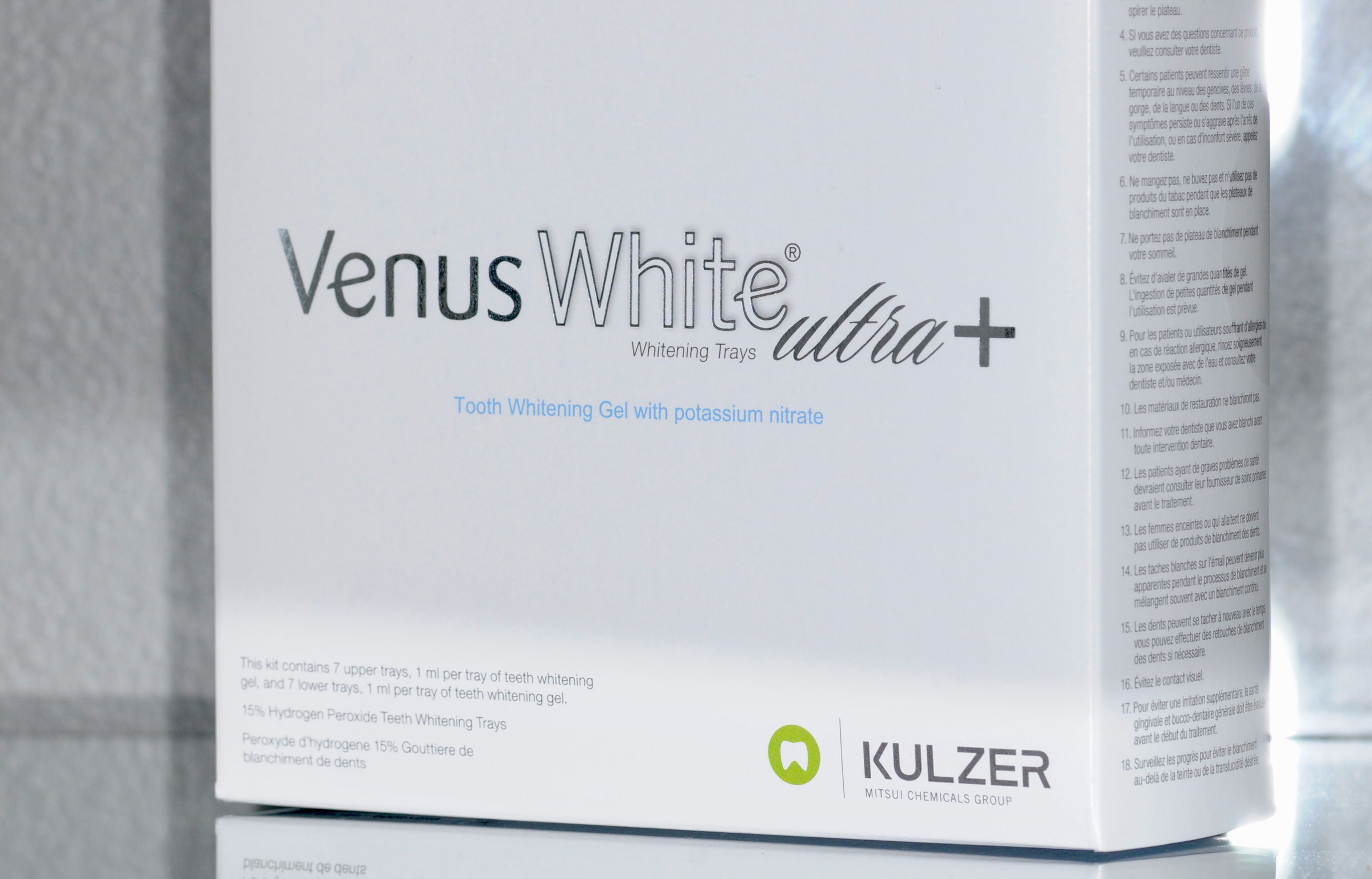
Lower cost and easy, quick application of the strips. In our practice, we recommend Venus white strips. These strips contain 15% hydrogen peroxide with potassium nitrate, which helps to decrease sensitivity. These strips are applied for 20 minutes per day for 7 days.
Benefits of custom take-home kits:
Custom trays are fitted for an even distribution of the gel for all of the teeth. For our take-home kit, we recommend Philips Zoom Nite White. This gel contains 16% carbamide peroxide with amorphous calcium phosphate, fluoride and potassium nitrate. Calcium phosphate and fluoride help to restore the enamel. Potassium nitrate helps to decrease sensitivity.
The expertise of a prosthodontist ensures a guided and effective teeth whitening journey, minimizing the risk of complications and enhancing the overall success of the process.
Consultation and Evaluation
Why It’s Important to Consult With a Prosthodontist
When pursuing a whiter and brighter smile, professional guidance is crucial to navigating the complexities of teeth whitening, ensuring a safe and effective outcome. A prosthodontist brings expertise in restorative dentistry, uniquely positioning them to assess and address the nuances of each patient’s oral condition.
The Initial Assessment and Examination
Oral Health Evaluation:
The first step in the consultation process involves a comprehensive oral health evaluation. Your prosthodontist will assess the overall health of your teeth and gums, identifying any existing issues that may impact the whitening process. This evaluation ensures that the chosen whitening method aligns with your oral health, mitigating potential complications.
Assessment of Existing Restorations:
We will also consider existing dental restorations, such as crowns or veneers. Unlike natural teeth, these restorations do not respond to whitening treatments. Understanding the presence and condition of restorations enables the prosthodontist to tailor your whitening plan, ensuring uniformity in the final tooth color.
Identification of Contraindications:
The consultation will include a thorough review of your medical history to identify any contraindications to teeth whitening. Certain conditions may impact the whitening process or harm oral health. Your prosthodontist will use this information to devise a safe and effective treatment plan, minimizing potential adverse effects.
Customized Treatment Plans
Tailoring Treatments to Your Needs
Severity of Discoloration:
The first step in creating your personalized treatment plan involves assessing the severity of discoloration. We will consider the nature and extent of stains on your teeth, allowing us to tailor the whitening approach effectively to address specific concerns. This individualized assessment ensures that the chosen treatment aligns with the unique characteristics of your teeth.
Your Preferences:
Understanding your preferences is integral to the customization of your treatment. When teeth are severely discolored, a combination of composite resin bonding and/or veneers may be used with a whitening treatment to achieve the desired result. In these situations, your input guides the selection of the most suitable treatment. This personalized approach enhances efficacy and ensures that you are comfortable and confident in your chosen path to a brighter smile.
Discussion of Potential Risks and Side Effects
As part of the comprehensive consultation, your prosthodontist will engage in a transparent discussion about potential risks and side effects associated with teeth whitening. This open dialogue allows you to make informed decisions, considering anything related to tooth sensitivity or gum irritation.
Custom Take-Home Teeth Whitening Kits
What Are Custom Take-Home Kits?
Custom Take-Home kits are comprised of two components:
- Custom-Fitted Trays: Take-home teeth whitening kits, prescribed by your prosthodontist, feature custom-fitted trays as a critical component. These trays are made to precisely fit the contours of your teeth, ensuring even application of the professional-grade whitening gel. The custom fit enhances the effectiveness of the whitening process and minimizes the risk of the gel contacting the gum tissues.
- Professional-Grade Whitening Gel: The prescribed take-home kits include professional-grade whitening gel. This specialized gel works in synergy with custom-fitted trays to penetrate the enamel effectively and target intrinsic and extrinsic stains. The professional-grade nature of the gel ensures a controlled and safe at-home whitening experience.

Proper Usage Instructions
- Duration and Frequency: Your prosthodontist provides clear instructions on the duration and frequency of using the take-home whitening kit. The recommended duration of wear and the frequency of application are tailored to your individual needs, considering factors such as the severity of discoloration and your oral health. Following these instructions diligently is essential to achieving optimal results without compromising safety.
- Monitoring Progress: Monitoring the progress of your at-home whitening is a collaborative effort between you and your prosthodontist. Regular follow-up appointments may be scheduled to assess the changes in tooth color and adjust the treatment plan if necessary. This proactive approach ensures that the whitening process aligns with your expectations, allowing for modifications to the treatment plan based on your progress.
Over-The-Counter White Strips
What Are Over-The-Counter White Strips?
- Over-the-counter white strips are ultra thin clear strips that mold securely around the teeth. These strips contain pre-filled 15% hydrogen peroxide to eliminate stains and whiten teeth.
Proper Usage Instructions
- Duration and Frequency: Your prosthodontist provides clear instructions on the duration and frequency of using the over-the-counter white strips. Each kit includes 7 upper and 7 lower pre-filled trays. Trays are applied once per day for 15-20 minutes, for up to 7 days. After use, the thin trays are disposed of.
- Monitoring Progress: Monitoring the progress of your at-home whitening is a collaborative effort between you and your prosthodontist. Follow-up appointments may be scheduled to assess the changes in tooth color and adjust the treatment plan if necessary.
Post-Whitening Maintenance and Care
After the whitening treatment, your prosthodontist will recommend long-term after care strategies for maintaining your white new smile.
Oral Hygiene Practices
- Brushing: Maintain a routine of brushing your teeth twice daily with a fluoride containing toothpaste, using a soft-bristled toothbrush to prevent gum recession. The Sonicare electric toothbrush with the Sonicare Sensitive brush heads are an excellent combination for daily use.
- Toothpaste: Toothpastes containing baking soda are great for maintaining white teeth. Baking soda is a gentle abrasive, biocompatible, acts as an acid-buffering agent, and possesses antibacterial activity. Baking soda is also compatible with fluoride.
- Flossing: Incorporate daily flossing to remove plaque and food particles between teeth. This not only helps to maintain excellent oral hygiene but also helps to maintain the tooth surfaces between your teeth.
Dietary Recommendations
- Limit Pigmented Foods and Beverages: Moderation of staining foods like coffee, tea, red wine, and dark berries is advised. Rinse your mouth with water after consumption. You can also use a straw when consuming staining beverages to bypass your teeth!
- Increase Water Intake: Drinking water aids in rinsing away staining particles after consumption.
Periodic Follow-up Appointments
- Monitoring Oral Health: Regular check-ups with your prosthodontist are necessary for monitoring oral health and assessing the effectiveness of the whitening treatment.
- Adjusting Treatment Plans if Necessary: Adapt whitening plans based on changes in oral health. Proactive adjustments, additional in-office treatments, or modifications to at-home regimens may be recommended to maintain results.
Addressing Sensitivity and Side Effects
Teeth whitening procedures, while effective, may lead to specific side effects. Understanding and addressing these potential issues ensures a comfortable and successful teeth-whitening experience.
Potential Side Effects of Teeth Whitening
- Tooth Sensitivity: One common side effect is increased tooth sensitivity, especially to temperature variations.
- Gum Irritation: Some individuals may experience gum irritation during or after whitening.
Strategies for Minimizing Discomfort
Use of Desensitizing Agents:
- Toothpaste: Switch to a toothpaste designed for treating tooth sensitivity. Toothpastes that contain potassium nitrate or biosilicate particles can be used daily to alleviate tooth sensitivity.
- Desensitizing Agents: Your prosthodontist may recommend a desensitizing agent that can be applied in the dental office for more moderate to severe tooth sensitivity.
Adjusting Treatment Intensity:
- Reduced Treatment Frequency: Space out whitening treatments or reduce the duration to allow teeth to adapt to the whitening treatment. This can minimize sensitivity.
- Lowering Whitening Concentration: If sensitivity persists, a lower concentration whitening agent can be used for the treatment.
In Conclusion
In conclusion, professional teeth whitening offers a clinically supervised, effective, and tailored approach to achieving a brighter smile. With the expertise of a prosthodontist, the benefits extend beyond cosmetic enhancement to encompass personalized care, minimal side effects, and long-lasting results.
If you’re wondering whether it’s time for a smile makeover, and considering teeth whitening, the advanced knowledge and specialized expertise of our prosthodontic team at Geach Dental, located in Downtown Los Angeles and Laguna Niguel, Orange County, are here to help ensure you get the attractive and confident look you deserve.
You’ll receive the personalized treatment you deserve in a comfortable environment. We’ll make sure you understand your teeth whitening options as well as all of the risks and benefits. Time will be spent to make sure that you are 100% comfortable with the plan we agree on.
To take the first step towards whiter teeth and a brighter smile, simply call us today at (213) 622-3339 or click here to schedule a consultation. Your dental wellness is our top priority and your journey towards a youthful, more attractive smile starts here!
References
- Vaz, et al. Inflammatory response of human dental pulp to at-home and in-office tooth bleaching. J Appl Oral Sci. 2016;24:509-517.
- Carey, C.M. Tooth whitening: What we now know. J Evid Based Dent Pract. 2014;14:70-76.
- da Rosa et al. Effectiveness of Whitening Strips Use Compared With Supervised Dental Bleaching: A Systematic Review and Meta-analysis. Operative Dentistry. 2020;45(6).
- Epple et al. A Critical Review of Modern Concepts for Teeth Whitening. Dentistry Journal. 2019;7(79).
ABOUT THE AUTHOR: Meet Dr. Adam Geach, distinguished prosthodontics specialist and owner of Geach Dental. His dental education includes Harvard School of Dental Medicine and the University of Connecticut, where he earned a D.M.D. and M.D.Sc. in Prosthodontics, respectively. Dr. Geach holds Diplomate status with the American Board of Prosthodontics, underscoring his exceptional expertise in dental care.
At his clinics in Los Angeles and Laguna Niguel, Dr. Geach offers a wide range of services, from cosmetic treatments to full-mouth reconstructions, all delivered with a focus on personalized patient care.Take the first step toward your ideal smile and improved oral health by clicking here.